by Dot Cannon
“Who’s ready for more Virtual Medicine?” asked Cedars-Sinai Director of Health Services Research Dr. Brennan Spiegel on Thursday morning.
He paused for a second.
“Who whooped?”
The sold-out crowd of 430 registered attendees was more than ready for Day Two of Cedars-Sinai’s second Virtual Medicine conference, in Los Angeles.
During Day One, they’d already explored numerous aspects of patient-centered medical virtual reality.
Sessions had included talks on VR’s use in mental health professions, pediatrics, and some of the feasibilities, and obstacles, of scaling medical VR to make it an everyday practice.
Now, Dr. Melissa Wong, Maternal Fetal Medicine Fellow at Cedars-Sinai, took the stage. Her topic: “Virtuo-Birthing: Experiences Using VR to Ease Labor Pain.”
Three questions
“I think we need to start by asking ourselves, ‘why does it matter?'” she began.
“It may come as a surprise to some of you, but labor hurts.” The audience laughed.
Dr. Wong told the audience that the pain level of labor was about at the same level as having a digit amputated. “But whenever you have that digit amputated, you don’t then take that digit, weep with joy and then give it a name,” she observed.
Dr. Wong explored the non-epidural alternatives which women have tried, to alleviate labor pains. Among the areas she named: aromatherapy, massage and acupressure.
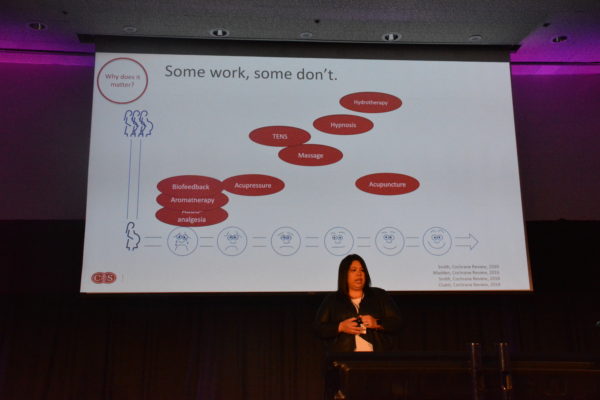
Dr. Wong’s graph showed acupuncture as the most effective alternative. Close behind it were hydrotherapy and massage. Aromatherapy, biofeedback and audio analgesia, she said, did very little.
So, how did virtual reality stack up?
Dr. Wong shared the results of a University of Michigan study, VRAIL, which involved 28 women. Half of the women in the research group, she said, were immersed in a virtual-reality experience of a swimming manatee for ten minutes, then had no intervention for ten minutes.
The main conclusion, Dr. Wong explained, was that, among the women using virtual reality, the labor pains diminished during the VR experience.
However, the study had limitations. One woman had chosen to leave the research group before the study ended. In addition, there were questions about the crossover design, and the fact that the VR experience lasted only ten minutes.
Dr. Wong continued her talk by looking into two additional questions: “What do we know so far?”, and “What are we working towards, in the future?”
Obstetrics plus VR: additional aspects
The next study she shared appeared to raise some questions about the efficacy of medical VR in one area.
Displaying a slide of episiotomy repair, she explained that one study had been done during which women received VR during the procedure.
The result? During the repair, Dr. Wong said, the group experiencing virtual reality actually experienced more anxiety. After removing the headsets, their anxiety levels dropped.
“It’s unclear why they had more,” she commented.
Later in her presentation, Dr. Wong referenced current antepartum research at Melbourne, Australia’s Monash Medical Centre. Researchers, she said, are currently trying to “flip” babies from breech to a normal delivery position.

Despite the obvious discomfort of the procedure, Dr. Wong pointed out that the patient appeared very relaxed due to being “immersed” in the medical VR.
In the postpartum area, she said, the most interesting work was happening around breastfeeding.
“Pumping is literally your brain releasing oxytocin to stimulate letdown,” Dr. Wong said.
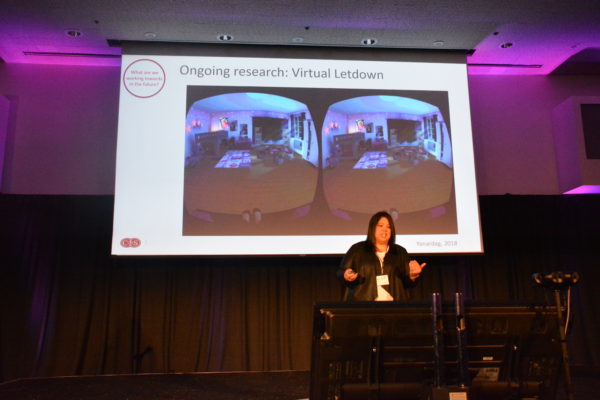
And that stimulation, apparently, may be done virtually.
“An MIT woman’s baby, Ada, stopped latching,” Dr. Wong explained. So, a subsequent hackathon addressed the problem.
Hackers created VR to show the woman virtual images of her nursery–and her baby–to stimulate milk flow! MIT currently has a research study to determine the results.
Meanwhile, Dr. Wong said, Cedars-Sinai continues to research the use of VR to reduce labor pain.
“We recruited 40 women,” she explained. These subjects will be experiencing their first pregnancy, be in the first stage of labor and have pain ratings between four and seven. Once they go into labor, in addition to the VR, the subjects will hear messages, relevant to labor. The goal: to prove a reduction in pain scores, using VR experiences that last up to thirty minutes.
“The recruitment’s completed, and the analysis is forthcoming,” Dr. Wong concluded.
“Unrealistic” expectations…
“The idea that you should have zero pain has become an ideal norm,” said Cedars-Sinai Orthopedic Trauma Surgeon Dr. Milton Little.
“…That’s somewhat unrealistic.”
During his presentation, “Make No Bones About It: VR Helps Orthopaedic Pain”, Dr. Little referenced the current opioid epidemic.
“We’re the third highest prescriber of opioids in medicine,” he said, of the orthopedics field.
In addition to the potential for opioid addiction, he added, use of pain-relief drugs presented other problems.
“A pharmacist may say, ‘you’re through with your medications too soon’ (and refuse to renew a prescription),” he said.
…and unexpected joy
Dr. Little told his audience of Cedars-Sinai’s recent research with 54 surgical orthopedic patients, to determine the effectiveness of virtual reality in pain reduction. Among the reasons for their surgeries: broken bones, stiffened joints and joint replacements. Patients were divided into two groups.
“What we do know, is that every patient is different,” Dr. Little said. “So we compared a 3D VR experience, utilizing a headset at least three times a day, to a two-dimensional AV experience.”
The results? No significant change appeared in pain levels either prior to, or during, the patients’ surgeries, in either group. The primary outcome was a significantly lower increase in pain scores among the VR cohort following surgery. (Dr. Little explained that an increase in pain scores is to be expected, after a surgical procedure.)
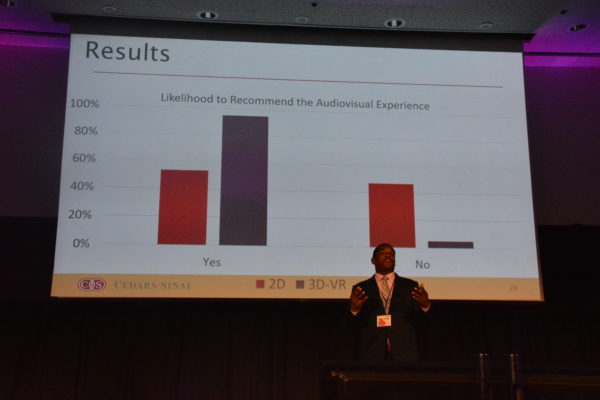
However, when patients in both groups were asked if they’d recommend their medical-distraction experiences, 90 percent of the patients who’d used VR said they would. By comparison, more than 50 percent of the patients using 2D experiences said they would not recommend them.
Dr. Little said that particular study had limitations–including limited ability to track patients’ usage, and a “technology gap” among some who were uninterested in the VR. However, Cedars-Sinai currently has another study in the recruitment stage.
“We will have over 120 patients enrolled by the end of April or May,” he said.
While not measurable elements, Dr. Little said he’d seen other benefits to the use of medical virtual reality. Patients using the VR experienced no side effects. And in addition, the technology brought an unexpected component to their hospital experience: happiness.
“If you can bring them joy, …that’s a big deal,” Dr. Little commented. “Every day, we have to deal with patients who have sustained a fracture. (Their injuries will keep them from doing the things they love.) So the future for us is, how do we make those experiences better for our patients?”
The challenges of scalability
Some of the obstacles facing medical VR implementation were the focus of Firsthand Technology Founder and CEO Howard Rose’s presentation.
“‘Cool’ and ‘Glow’ are in hospitals right now,” he said, referring to two of his company’s VR pain relief applications. “One of the real challenges of doing this, they contacted us (and) wanted it (at) bedsides 24/7.”
With the applications available around the clock, he said, sterilization was an issue. In addition, visitors could appropriate the headset.
“What if Johnny goes over (and decides to play)?” he asked.
“(It’ll need to be) wireless. We’re not there yet, but almost.
“I think the future we’re going to, is a really nice, high-powered machine, off in the closet, sending signals to that headset.”
And there was also the issue of getting patients–and hospital staff–accustomed to use.

“We reach for our phone reflexively,” he said. “But we don’t have that same sort of reflex, to reach for VR.”
Scaling the system
Cost reimbursement, Mr. Rose continued, was another problem.
“I’m a developer. I’ve been doing this for many years,” he continued.
“It’s not just the ability for me to develop ‘Cool’ and ‘Glow’. I have to be able to deliver it.”
Part of that delivery problem was payment.
“Hospital budgets take 18 months (to process payment),” he said.
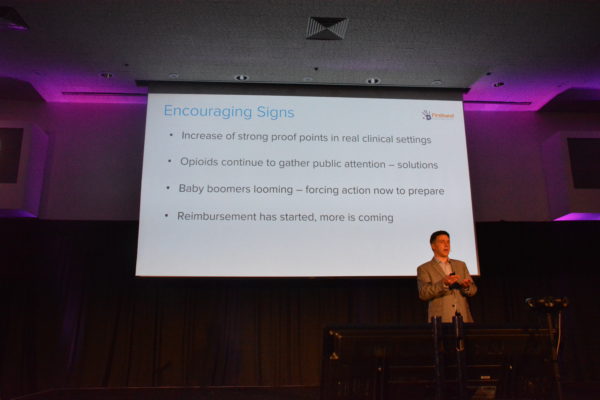
But, Mr. Rose continued, he was seeing a number of indicators that medical VR use would continue to grow.
The “tipping point”, he said, would be 30 percent of use of medical VR, in hospitals. And he encouraged the audience to think in terms of balance.
“You want a limited number of applications, you want enough and you want quality. Offering (VR) 24/7 is not necessarily better.
“I think the word ‘distraction’–we need to move beyond (that) concept, we need to (create) activation.”
VR’s “superpower”
“A few months ago, I asked (my eight-year-old son) Nathaniel, ‘if you could have any superpower, what would it be?” said Dr. David Rhew, Chief Medical Officer and Vice-President and General Manager of Enterprise Healthcare, at the start of his keynote.
“He said, ‘I’d love to be able to transport.’ That really is the genesis, the foundation of what VR is. You’re teleporting yourself to another place.”
Dr. Rhew outlined the exciting ways extemded-reality technology –along with AR and VR–could be used for “not just fun, but exciting things in health care.”
Just one of those was a University of Wisconsin study, which “virtualized” a program to treat addiction.
This is an app, which senses a user’s location, asks for a “weekly check-in”, and offers a chance to text a friend if, for example, the user is near a bar.
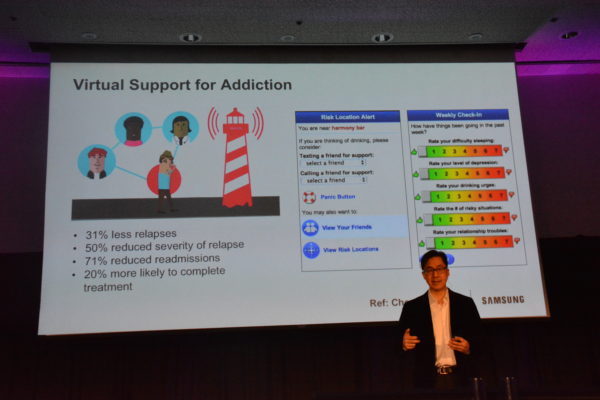
According to Dr. Rhew’s slide, this virtual support decreased both relapses, and the severity of relapses, among alcoholics in the research study group. It also cut their readmissions for alcohol addiction by more than two-thirds!
“There is an element here of (improving) the ability for people to have 24/7 support,” Dr. Rhew commented.
Virtual tools, real-world results
And his keynote would include even more exciting ways of using technology “for good” in the healthcare industry.

Next, Dr. Rhew showed the audience how virtual reality, plus an exoskeleton, equaled using XR to “trick” the brains of patients with spinal-cord injuries. An implantable device enabled them to regain the use of their legs!
“We are now working with the Christopher Reeve Foundation, to implement these technologies,” Dr. Rhew said.
Later on in his presentation, he would also show a VR session which patients do, daily, to improve “lazy eye” syndrome. And a big area, he said, was getting technology-averse patients to use VR.
“Even the current seniors, over 65, are starting to use technology,” Dr. Rhew said. And one such use, he continued, was reminiscence therapy for dementia patients.

“You put the VR headset on, they’re now back in their hometown. They’re in their own home.
“They’re in Paris, where they got engaged.”
A final exciting area in the medical use of VR which Dr. Rhew explored was its potential to restore vision to patients with macular degeneration. Currently, he said, 100 ophthalmologists are using the technology, by a company called Iris Vision.
“There’s actually a secondary part of the eye,” he said. “If only we could latch onto that, we’d be able to see again.”
Beyond description
Like Cedars-Sinai’s inaugural “Virtual Medicine” conference in 2018, “VMed19” was incredible. No single post could do it justice.
Stand-out favorites of the day, though, included “The Bicycle of the Mind”. This was a presentation by Patient Advocate Harmon Clarke.

Last year, Harmon was one of several patients participating in a panel about their experiences using medical VR. This year, he presented his experience to the audience independently.
Harmon explained that he had first had symptoms, at the age of 16, of debilitating Crohn’s disease. Confined to a hospital room and rapidly losing weight, he thought he was going to die. Horrific pain left him in tears–but pain medications made his brain so “foggy” that he couldn’t think straight.
Then, one day, Dr. Spiegel showed up at his hospital room with a VR headset.
“I’m just like, really, VR? Give me my pain meds. Get out of here,” Harmon said.
But the virtual reality proved not just effective–but dramatically so.
Harmon told the audience that he was now a yoga instructor, had traveled worldwide and was just about to leave for Florida, on tour with a musical in which he sings and dances.

“This device saved my life,” he said.
And Harmon would share his talents with his listeners–not only with an original song he’d written about achieving his dreams…

…but with a “rap” duet with Dr. Spiegel!
Forthcoming was a “Patient Panel” that completely deserves its own post. So, it’s going to get one!
And, suffice it to say, for now, the afternoon would be equally amazing as “Virtual Medicine 2019” continued.
This is Part One of a series.
